TYPHOID FEVER (ANTRIKA JWARA):-
👉🏻 Introduction:-
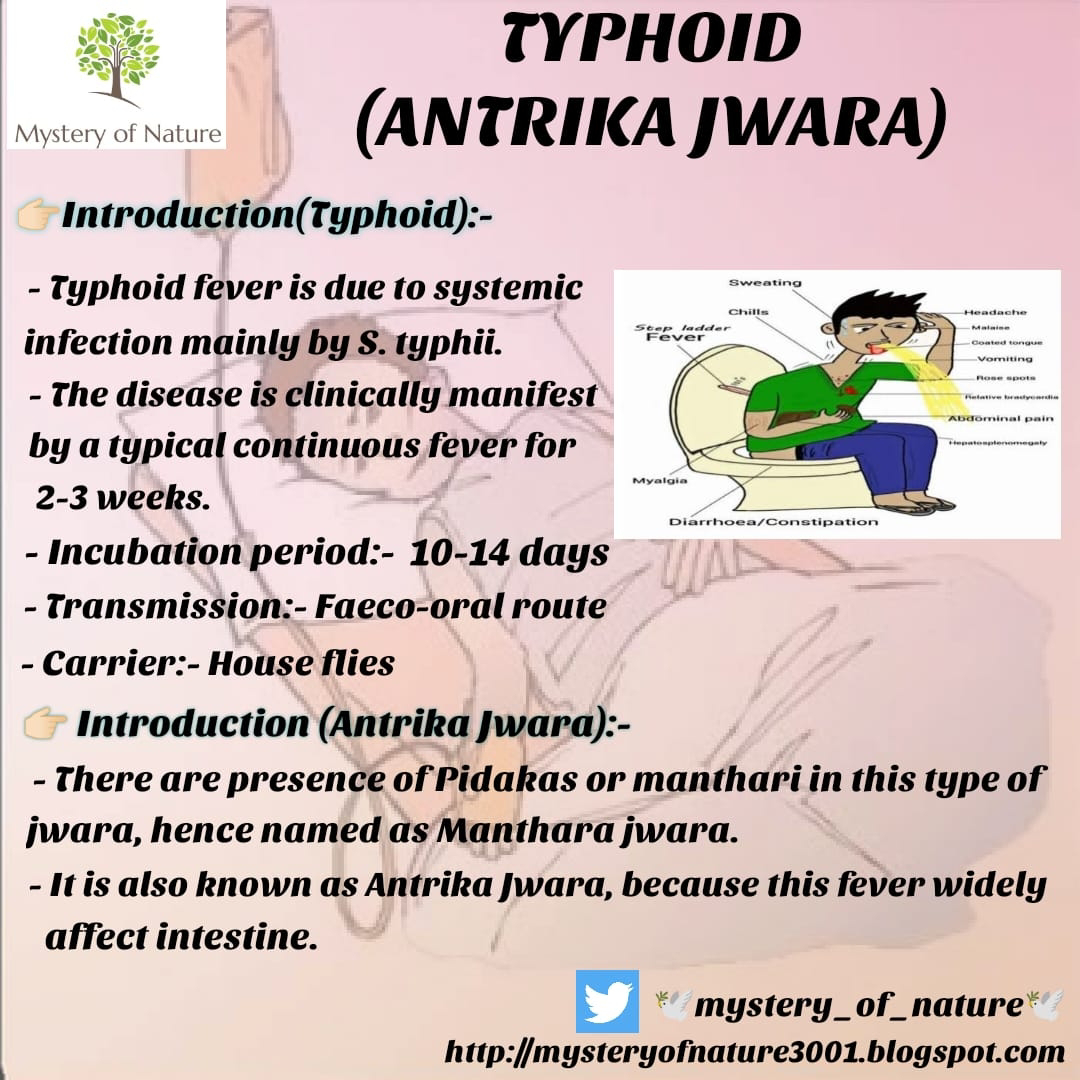
- Typhoid fever is due to systemic infection mainly by Salmonella typhii.
- The disease is clinically characterised by a typical continuous fever for 2-3 weeks.
- In Ayurveda it is correlated with 'Enteric fever, आन्त्रिक ज्वर or मन्थर ज्वर.
👉🏻 Causitive organism:-
- Salmonella typhii (Gram -ve, anaerobic bacilli)
👉🏻 Incubation period:-
- 10-14 days
👉🏻 Source of infection:-
√ The primary source of infection are:-
- Contaminated food, milk and water
- Pollution of drinking water supplies
- Open air defecation and urination
- Low standards of food
- Low personal hygiene and health ignorance
√ Transmission :- Feco-oral route
√ Carrier :- House flies
👉🏻 Risk factors:-
- Typhoid fever is a serious worldwide threat and affects about 27 million or more people each year.
- The disease is established in India, Southeast Asia, Africa, South America and many other areas.
- Worldwide, children are at greatest risk of getting the disease, although they generally have milder symptoms than adults do.
√ If you live in a country where typhoid fever is rare, you're at increased risk if you:-
- Work in or travel to areas where typhoid fever is established
- Work as a clinical microbiologist handling Salmonella typhi bacteria
- Have close contact with someone who is infected or has recently been infected with typhoid fever
- Drink water polluted by sewage that contains Salmonella typhi.
👉🏻 Pathogenesis:-
- Due to contaminated food, milk and water, salmonella typhi bacilli enters and reaches to the intestine.
- In intestine, it penetrate the mucosa of intestine and reaches to the intestinal lymphatic through peyer's patches.
- From peyer's patches it enters in blood stream.
- In blood stream, the bacteria is disseminated throughout body via blood and intracellular multiplication occurs.
- The organism enters intro the blood stream and producing bacteremia when all organs are repeatedly exposed.
- It affect different body organs.
• Brain:- Encephalitis
• Heart:- Cardiac failure
• Lungs:- Pneumonia, Bronchitis
• Liver:- Hepatomegaly
- 3rd week is most critical phase.
👉🏻 Clinical features:-
✓ 1st week (Prodromal stage):-
- Mild fever (99-100° F)
- Malaise
- Headache
- Generalised bodyache
- Cough
- Sore throat
- Often with abdominal pain
- Constipation
- Stepladder fashion (pattern) fever
- Relative lynohocytosis with leucopenia.
✓ 2nd week:-
- High grade fever (Temperature gradually rise upto 107° F)
- Fever reaches at peak and patient looks toxic appearing exhausted.
- Marked abdominal tenderness
- Mild hepatospleenomegaly
- Relative bradycardia
- Diarrhoea:- Pea soup like stool
- Red rose spots or red spots may seen on chest and abdomen, disappeared within 2-3 days
- Constipation:- Caused by swelling on lymphoid tissue around ileocaecal junction.
✓ 3rd week (Stage of complication):-
- Intestinal perforation and haemorrhage
- Meningitis
- Pneumonia, bronchitis
- Cardiac failure
- Encephalitis
👉🏻 Diagnosis:-
- CBC:- Leucopenia - 1st week
- Antigen:- WIDAL test - 2nd week
- WIDAL test detects O and H Antigen of Salmonella typhii.
- Culture:- Stool, Urine - 3rd and 4th week
- Typhi DOT:- More accurate than WIDAL, shows early result on 2nd or 3rd day
👉🏻 Diffrential diagnosis:-
- Pneumonia
- Dengue fever
- Malaria
- Cerebrospinal fever
- Tuberculosis
- Relapsing fever
👉🏻 Management:-
1) For prevention:-
- Providing clean water to public
- Proper excreta disposal
- Protection of water from contamination
2) For treatment:-
- Bed rest
- Fluid management:- Oral / IV
- Antibiotics
- Steroid therapy
- Surgical intervention:- 3-5%
✓ Antibiotics:-
1. Chloramphenicol:- 3-4 gm/day
(Continues with 2gm/day for 18 days)
2. Amoxicillin:- 4-6 gm/day (In 4 divided doses)
3. Ciprofloxacin:-:500-750mg BD
4. Ampicillin
5. Ceftriaxone:- 75 mg/kg/day
6. Cefexine:- 400mg BD
7. Azythromycin:- 1gm, once in a day for 5-7 days
✓ Steroid:-
1. Dexamethasone:- 1mg/kg every 6hrs
💫 ACCORDING TO AYURVEDA:- ANTRIKA JWARA Or MANTHARA JWARA
👉🏻 Introduction:-
- There are presence of Pidakas or manthari in this type of jwara, hence named as Manthara jwara.
- It is also known as Antrika Jwara, because this fever widely affect intestine.
- In this type of Jwara, all tridosha lakshana are present.
- In modern it is correlated with Typhoid fever.
👉🏻 Samanya Nidana:-
• "बह्वध्व क्लान्ततनवस्तथाऽनश्नकर्षिताः।
दुर्गन्धिपूर्णभूमौ वा नित्यमेव निवासिनः॥
आंत्रिककेत्यभिधानं चापरमस्यैव कथ्यते।
सामस्य कारणं प्रोक्तं विशिष्टं तु निगद्यते॥"
(मा.नि. परि. मंथर ज्वर 1-4)
- Ati margagamana
- Ati upavasa
- Durgandha purna, dushita sthana nivasa
- Intake of food and drinks contaminated with dushita mala etc.
👉🏻 Vishista Nidana:-
- Agantuja karana:- Bacterial infection
👉🏻 Samprapti:-
• कीटाणवो बेसिलस टाइफोसस नामकाः ।
दण्डाकाराः कृतावासा रक्ते मूत्राशये मले।
स्वेदे पित्ताशये प्लीह्नि पिडिकास्वान्त्रिकव्रणे।
जनयन्ति नृणां देहे ज्वरं प्रोक्तं विशेषतः॥"
(मा.नि.परि.)
• मलमूत्रस्वेदजात दोष संसर्ग दूषिते।
भक्ष्यपेयादिभिद्रव्यैर्नाना संक्रमणकारणैः ॥
लक्ष्येत यदि रक्तस्थस्रावो भिन्नान्त्रता तदा॥"
(मा.नि.परि.मन्थर ज्वर 7/11)
- Due to nidana sevana and Bacterial infection (Jivanu sankramana) jivanu (bacteria) enters into antra (intestine).
- After entering, it produces swelling in sntra granthis.
- Due to swelling doshas, rasa and rakta dhatu exists in intestine are aggravated and producing kshata (injury) to the intestine.
- After some time kshata (injury) increases and produces chhidra in antra (perforation of intestine) and causes continuous blood flow in intestine.
- It creates Manthara (antrika) jwara, and this condition is Asadhya when antra is perforated.
👉🏻 Samprapti ghataka:-
- Dosha:- Tridosha
- Dushya:- Rasa, Rakta
- Srotasa:- Annavaha, Rasavaha
- Srotodushti:- Sanga
- Adhisthana:- Antra
- Swabhava:- Chirakari
- Sadhyasadhyatva:- Kruchrasadhya
👉🏻 Purvaroopa:-
• शिरोव्यथा स्यादरुचिस्ततोऽरतितमोऽवसादौऽपि च बिड्बद्धता।
सप्ताहपर्यन्तमिति स्फुटास्फुटं ज्वरेऽग्ररुपं नियंत सदाऽऽत्रिके॥
(मा.नि.परि.)
- Shirovyatha (headache)
- Aruchi (anorexia)
- Restlessness
- Darkness in front of eyes
- Depression
- Malabaddhata (constipation)
👉🏻 Lakshana (Clinical features):-
• तदग्ररुपं च ततोऽष्मेऽहनि भवेदभिव्यक्तिमवाप्यलक्षणम्।
ज्वरोऽथ नित्यं क्रमश: प्रवर्द्धते सहापरैमर्थरेकऽत्र लक्षणैः ।।
भवेत्तदा तु ज्वरजाप सीमा चतुर्भुतं पञ्चमुतं शतं वा॥
उपद्रवसमाधिक्यं सप्ताहितं सेविन:।
(मा.नि. परिशिष्ट)
- It is similar to Pittolbana Sannipataja jwara.
- It is explained by Acharya Gananath sena in Siddhanta nidana, which are similar to Typhoid fever in modern.
✓ 1st week:-
- Jwaradhikya (Hyperpyrexia)
- Pleehavriddhi (Spleenomegaly)
- Jihva malina evum rakta varna (Tongue coated and reddish)
- Adhmana (Flatulence)
- Vibandha (Constipation)
- Red spots on neck, abdomen and chest area
✓ 2nd week:-
- Jwaradhikya (Hyperpyrexia)
- Pralapa (Delirium)
- Tandra (Drowsiness)
- Kasa (Cough)
- Furrowed tongue, dry with reddish coloration
- Durbalata (weakness)
- Mukhashosha (Dryness of mouth)
- Arati (Restlessness)
- Adhmana (Flatulence)
- Dicrotic pulse
- Blood mixed stool
👉🏻 Asadhya Lakshana:-
- Ati raktasrava (Excessive bleeding)
- Increased pulse rate
- Acute pain in abdomen
- Tendency of raised body temperature during morning hours and night
- Generalized peritonitis
- Excessive weakness
- Tremora in hands and feet
- Intestinal bleeding
👉🏻 Upadrava:-
- Antra kshaya (Intestinal tuberculosis)
- Vishaktata (Toxaemia)
- Raktasrava (Haemorrhage)
- Peritonitis
- Antra vidarana (Intestinal perforation)
- Vrukka Shopha (Nephritis)
👉🏻 Chikitsa sutra:-
- Firstly Langhana should be done for dosha pachana.
- In Sannipataja jwara, when there is ugra vega of jwara; first treat pitta then treat kapha and vata dosha respectively.
• कफस्थानानुपूा तु सन्निपात ज्वरं जयेत्।" (च.चि. 3)
- In lakshana Manthara jwara is similar to Sannipataja jwara so its treatment should be done according to Kapha sthana
- Firstly done Kapha and Amadosha pachanaz then treat aggravated vata and pitta.
- In case of constipation sramsana aushadha should be used for koshtha shodhana according to Bala of rogi.
- In antra pradhaha sheeta, tikta and madhura rasatmaka dravya should be used.
- If Trishna present, then use Shadangapaniya.
- Pathya Palana
- Pushtikaraka, balaprada and supachya drava ahara should be taken.
👉🏻 Chikitsa:-
1. Samshodhana Chikitsa:-
√ Same as Sannipataja jwara treatment:-
a) Langhana
b) Swedana :- Baluka, Sandhava sweda, Snigdha sweda
c) Shirovirechana:-
- Trikatu churna pradhamana nasya
- Kataphala twak churna pradhamana nasya
- Shwara kuthara rasa nasya
d) Anjana prayoga
2. Samshamana Chikitsa:-
a) Rasa / Bhasma / Pishti:-
• Matra:- 125-250 mg
• Anupana:- Ushnodaka / Madhu
- Sutashekhara rasa
- Pravala pamchamrita
- Karpura rasa
- Ramabana rasa
- Yogendra rasa
- Bola parpati
- Navayasa lauha
b) Vati:-
• Matra:- 250-500 mg
• Anupana:- Ushna jala
- Madhurantaka vati
- Saubhagya vati
- Samshamani vati
c) Churna:-
• Matra:- 3-6 gm
• Anupana:- Koshna jala
- Sitopaladi churna
- Yavani shadava churna
d) Kwatha / Asava / Arishta:-
• Matra:- 10-20 ml
• Anupana:- Jala
- Chandanadi kwatha
- Mustadi kwatha
- Kiratadi kwatha
- Chandana kiratadi kwatha
- Lohasava
- Draksharishta
e) Anya yogas:-
- Lavanga:- 7
- Jatiphala:- 2gm
- Sunthi:- 2gm
- Ela:- 2
- Tulasi:- 5 patra
• These all should be added with 400 ml water and boiled until 50 ml is remained and given with madhu.
👉🏻 Pathya-Apathya :-
1) Pathya:-
- Ahara:-
Kurchika, dadima, draksha, munnaka, godugdha, mudga, yava manda, laja manda, Purana shali, peya, vilepi, patola, lavangodaka, Shadangapaniya etc.
- Vihara :-
Langhana, Vishrama, avoid vega dharana
2) Apathya:-
- Ahara :-
Guru, Abhishyandi, tikshna bhojana, pizza, burger, samosa, kachori, halva, malpuva etc.
- Vihara :-
Adhyashana, Vyayama, Vyavaya, Shrama, Chinta, Jagarana etc.